By Eleanor Tanno, M.D.
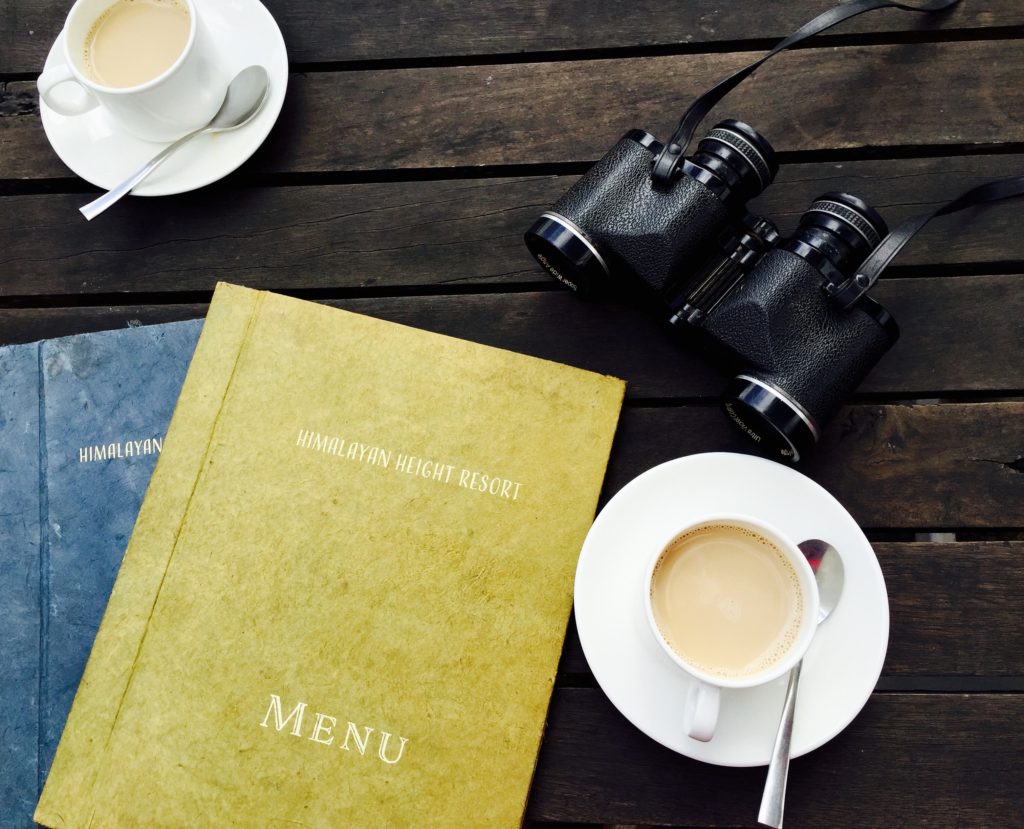
Naming your “medical wishes” for end-of-life planning can be a daunting task. If you are not familiar with the medical field, this is a tall order. I liken this to asking someone to choose a meal at a restaurant without a menu. How can you be expected to be familiar enough with medical interventions to be comfortable selecting what you do and do not want?
Below is an overview of the types of medical interventions at the end of life. This list is not exhaustive since much of the additional medical care depends upon your specific medical condition. However, these interventions are those that are offered when someone is really sick and is in critical care. These are the interventions that are often referred to collectively as “life support.” As always, if you are conscious and well enough to make your own medical decisions, your physicians will always defer to you for your medical decisions.
It is important that you discuss these interventions with your family and, specifically, your medical power of attorney (POA). You may even want to go ahead and specifically document them in your written advance directive.
What are the possible medical interventions at the end of life?
Here they are listed, but I will explain each one in more detail below:
- Cardiopulmonary resuscitation (CPR)
- Ventilation
- Antibiotics
- Blood transfusion
- Artificial nutrition
- Dialysis
The interventions up close
Let’s start from most straightforward, then move to the most nuanced.
Blood Transfusion
Blood transfusion – would you accept a blood transfusion to save your life or to make you feel substantially better? Contrary to common belief, most blood transfusions are not used in traumatic injuries, but are actually used for other causes of anemia (low blood counts). The anemia is most frequently from internal bleeding (often intestinal), chronic kidney disease, cancers, obstetrics/gynecological bleeding, and related to surgery.
The risks of contracting an infectious disease, such as HIV or hepatitis, from transfused blood is extraordinarily low now with modern screenings. Additionally, you are not “taking away” blood from someone else if your physician recommends you have a blood transfusion for your condition.
I usually advise people be open to accepting a blood transfusion unless you have a specific religious objection to taking blood.
Antibiotics
Antibiotics – In the event that you need antibiotics to treat a serious infection, would you want them? This seems like an odd question, but keep in mind some of the most peaceful deaths can be from an overwhelming infection. You may decide that if you are sick enough or old enough, you would forgo antibiotics and allow the infection to run its course.
Take the case of an elderly lady in a nursing home who has been admitted four times in the past six months with a common, severe, recurrent intestinal bacteria called C. difficile (“c-diff” in circles where it is well known). Each time she gets another C. diff infection and goes to the hospital, she returns to the nursing home weaker and weaker, with a lower quality of life. She may decide that if she gets very sick again, she would rather not be treated with antibiotics and rather pass away from the infection.
Antibiotics come in different forms. In the hospital, many of the most powerful antibiotics can only be given through an IV, not in the form of a pill. If you would like to do a trial of non-invasive antibiotics, you can opt for just oral antibiotics, but not IV antibiotics. Lastly, you can choose to allow oral and IV antibiotics. I typically advise patients to leave their options on this one, but talk to your POA about your end-of-life values.
Dialysis
Dialysis – if your kidneys fail and you are no longer able to filter your own blood from toxins naturally, would you want dialysis to act in place of the kidneys? Dialysis is a process where a machine hooks up to you through a large IV and takes blood out, filters it, and returns it to your body. To keep your blood sufficiently filtered, dialysis is usually performed about three times per week and takes four hours each time.
If you would like dialysis, would you just want it only in the short term in case your kidneys recover on their own, or would you want to be on it indefinitely if your kidneys fail? Keep in mind that death from kidney failure is generally a peaceful death.
Artificial Nutrition
Artificial nutrition – if you are not well enough to eat or drink on your own, would you want IV fluids and/or artificial nutrition to be used initially to sustain you, but then later to prolong your life? IV fluids are given through a standard IV in your arm. Artificial nutrition can be administered through a feeding tube into your stomach or through a large IV that is placed in one of the larger veins.
Near the end of life, if you are not conscious, you are not hungry or thirsty. There comes a point when these interventions just prolong your life without adding any quality. The feeding tube, in particular, can be uncomfortable and increase your risk of infection.
In the case of end-stage dementia, fluids and food refusal are part of disease. It can be very uncomfortable to feed these people after a certain point in their illness.
Ventilation
Ventilation – this is a question about how much support you want to offer your lungs if breathing becomes difficult. Scenarios where you might need help breathing are pneumonia, after a stroke, or in a systemic infection where you are delirious. Often times, the breathing support is temporary and buys time while the underlying condition is treated. For example, a breathing tube may be used in the case of pneumonia while antibiotics are allowed to work. I will get to the more permanent ventilator scenario a little later.
The respiratory support is generally upgraded in a stepwise fashion:
The first step when someone is short of breath would be minimally invasive options. These start with an oxygen tube under your nose, then a mask with oxygen flowing.
–>The next step is to use CPAP, then BiPAP, which are moderately invasive methods as they use masks with forced air into your lungs. These are generally not very comfortable, but no device is in your throat. An important distinction here is that in some hospitals, CPAP and BiPAP cannot be given on a regular floor and you need to be upgraded to the ICU to get these interventions.
–>The last, most invasive, breathing intervention is a breathing machine, or ventilator. In this case, a rigid tube is inserted down your trachea (windpipe) in a procedure called intubation. This tube is then connected to the ventilator. The ventilator pushes oxygenated air through the tube into your lungs with each mechanical breath. Because this is invasive and sometimes patients try to pull the tube out, they need to be sedated and in the ICU for the treatment. The hope is that the condition improves and the tube can come out, but not this is not always the case.
When discussing whether you would like respiratory support as part of your life support arsenal, you have the choice to do none or draw the line somewhere and not allow escalation. Consider that if you are already quite ill and with a low quality of life (for example, end stage lung cancer), you may choose to not enter this cascade of breathing support at all. Your doctors would make sure you are comfortable until you passed away.
Permanent Ventilator Situation
Generally, people who end up needing a ventilator enter the hospital without any breathing support and quickly deteriorate to needing one. The question becomes, how long to leave someone on the ventilator? As long as you are improving, you will not be removed from the ventilator. Your doctors will continue to give you more time and reassess frequently.
In the scenario where you are not improving, your POA will need to decide when, if ever, to remove the breathing tube and disconnect you from the machine. Of course, if you have an advance directive, that will guide them.
As far as timing of how long to leave a person on a ventilator, there is a big shift after two weeks because that is when you will need to be moved from a temporary ventilator to a permanent one. The machine is the same, but in the temporary case, you are connected to the machine through a breathing tube though your trachea (windpipe) that enters through your mouth. After about two weeks, the temporary tube causes too much damage in the throat and needs to be replaced with a more permanent tracheostomy (“trach”) tube. A tracheostomy is where the tube is surgically inserted through the neck to allow a permanent connection to the ventilator.
People who are permanently connected to a ventilator often live in long-term care facilities where they can be properly treated until they get better (rare) or pass away. In fact, a study looking at 126 patients who were placed on long term ventilators found that one year later, only 9% of patients were alive and independent without major limitations.
The permanent ventilator is what most people refer to when they say “I don’t want to live on a ventilator,” or “pull the plug,” but others might say “I want everything done to live as long as possible.” The beauty of an advance directive is that they remove this almost impossible decision from your POA because you have already decided for them.
Cardiopulmonary Resuscitation (CPR)
CPR is a procedure performed when your heart stops beating and you stop breathing. In other words, you have suffered a cardiac arrest and are dead. The goal of CPR is to restart your heart to get blood pumping again to your body. In the interim, chest compressions are used to manually compress the chest to pump blood from the heart through the lungs to the body. This provides oxygenated blood to your body, most notably your brain. Electrical shocks and drugs are also used in an attempt to restart the heart.
If you do NOT want CPR performed, you need to have an easily accessible Do Not Resuscitate (DNR) order signed by a physician. By default, if you do not have a signed DNR order, CPR will be attempted by EMTs/paramedics.
Since CPR is such a nuanced intervention, I have a separate article dedicated to the topic.